- What is a cervicogenic headache? If you suffer from headaches, you could be associated with the 15-20 percent of those who experience cervicogenic headaches (CGH). It’s characterized by pain stemming from a dysfunction in the neck joints. The most common patients around the age of 42, and women are 4 times more likely to be affected than men. Whatever degree the case may be, our safe and effective treatments – including exercises and stretches for cervicogenic headaches – are here for you on your road to recovery at Complete Care Physio.
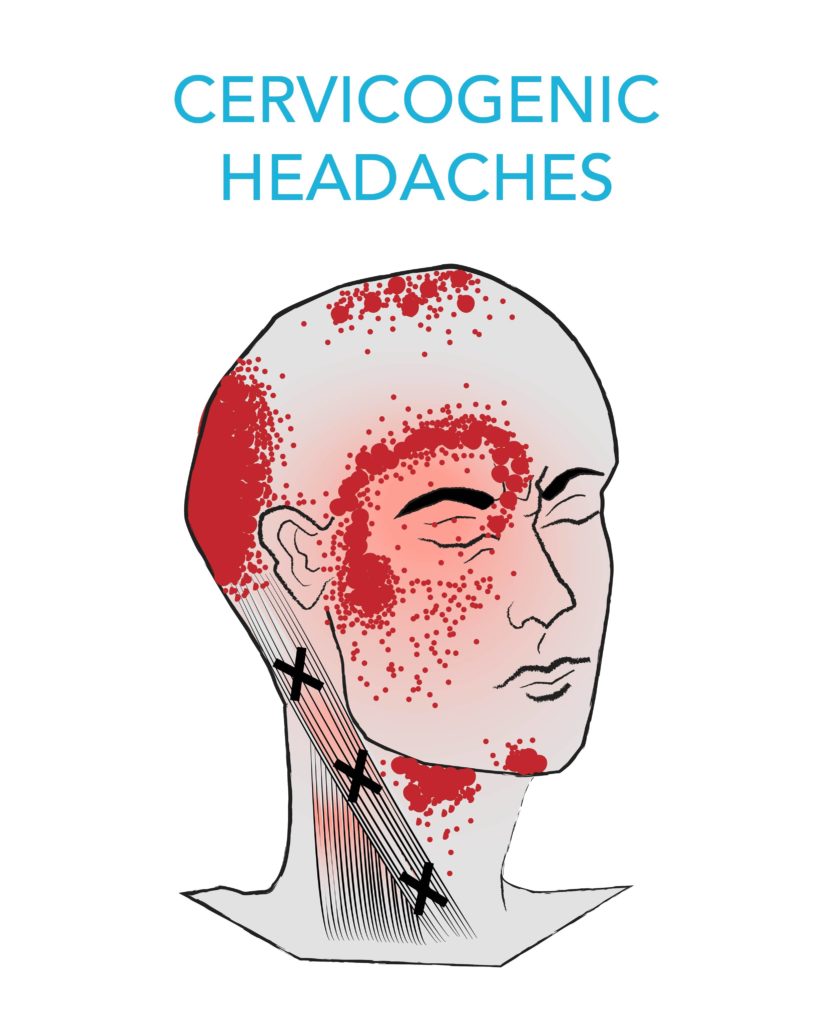
A cervicogenic headache (CGH) is classified as a secondary headache disorder, meaning the pain is a symptom caused by a source other than at the head. It can be referred to as one or a combination of dysfunctions to the muscles nerves, soft tissues and/or bones at the neck. In this case, it can be a result of chronic neck strain, inflammation or other traumas along the cervical joints, and is usually experienced unilaterally, or to one side of the head.
Causes
-
- What causes a cervicogenic headache? The source of the problem is due to a sensitised brainstem which radiates pain from the upper neck to the head and face areas. The trigeminocervical nucleus (TCN), along with the brainstem, is located in the upper three cervical spine and is important in the interaction of sensory nerves and the sensation of pain. Patients will experience cervicogenic headaches in the upper three cervical spine:
-
-
- Atlanto-occipital joint: at the base of the skull (O)-C1
- Atlanto-Axial joint C1-C2
- C2-C3
- or a combination of all 3 segments
-
- Who suffers from a cervicogenic headache? Most who suffer from CGH do not have history with acute neck trauma and pain is usually attributed to repeated neck distress. Over time, the injury develops as a result of poor neck posture. CGH caused by repetitive strain injury (RSI) can be caused through:
- building or painting jobs that require the head to be constantly held up or down
- neck protruding constantly during office work or desk jobs
- users who keep their neck forward while on their phone or computer
- Motor vehicle accidents
- A fall
- A blow to the head
- Any other whiplash injuries
Symptoms
- What do cervicogenic headaches feel like? The symptoms of a CGH are moderate to mild and intense pain. Patients will feel deep, unthrobbingas pain and indicate the location to be unilateral or occasionally bilateral (appearing on both sides of the head) disorder. It will start at the neck, and move towards the head and facial regions. Cervicogenic headaches can last from hours to days depending on severity, and come as irregular or constant attacks. Additionally, the headache will be triggered by neck movement and awkward posturing, and in some instances even through coughing and sneezing.
-
- Sharp pulsating pain near the eye, forehead, side or back of the head
- Vocal discomfort or difficulty swallowing
- Neck stiffness
- Nausea and vomiting
- Dizziness
- Lack of focus
- Can involve depression
Other signs of a cervicogenic headache include:
- How to diagnose a cervicogenic headache It may be harder to distinguish a cervicogenic headache with other common headache disorders such as a migraine or tension type headache. Although not formally validated, a tumor, fracture and infection should be considered. Patients who have endured a whiplash or concussion-like injury consequently suffering neck pain may develop a CGH. A headache appearing 3 months after the head injury may be associated with a cervical disorder rather than as a result of head or brain damage.
A major indication will be ipsilateral pain or pain more focused to one side at the neck, shoulder or arm, with a patient having trouble pinpointing a direct source. The pain will have fluctuating or continuous episodes of varying duration.
They will also recall altered and reduced neck motion. A trigger point may also be apparent at either the head or the neck. To ensure that successful recovery of a cervicogenic headache, cervical resolution to the area of the lesion will be needed through a variety of treatments.
- How do you treat cervicogenic headaches?
Since this type of headache is considered a syndrome, its treatment can vary for different people and relies on many different factors. Relief from cervicogenic headaches involves a multifaceted approach.Treatments for CGH can range from pharmacological (medications), physical therapy, exercise and surgical procedures.
Medical treatment:
In most cervicogenic headache circumstances, patients will find medication used as the only solution for pain relief, to be ineffective. Despite this, they can allow for increased recovery in addition to physical therapy and rehabilitation. Your physician will personally prescribe a pain medication at an initially low dosage to gradually increase your pain tolerance over 4 to 8 weeks. Frequent follow-ups are highly recommended.
Physical Therapy:
Any patient – no matter what age, gender or pain intensity that is experienced – can achieve relief and benefit from the manual and physical modes of treatment. This includes safe, drug- and surgery-free osteopathic procedures which our physiotherapists can provide. Osteopathy services are manual craniosacral, strain, tissue work and gentle muscle energy techniques which can help ease the tension and bring mobility back. Some non-pharmacological treatments to well manage the cervicogenic headache can include Deep Tissue and Craniosacral Massage Therapy and controlled stretches for cervical traction.
Surgery:
It is not generally advised to perform occipital procedures and/or a neurectomy, dorsal rhizotomy, joint fusion, nerve “release” and microvascular decompression without substantial radiological evidence and past medical history in which surgery is needed. Though a number of these surgical processes have had substantial results, only temporary relief of cervicogenic headaches have been accomplished.
Any patients who believe they are suffering from cervicogenic headaches are advised to seek professional help. One of the most successful options to solve cervicogenic headaches involve an individualized direct approach, which your physicians at Complete Care Physio are dedicated to delivering.
If you are interested in Brampton and Hamilton (East Hamilton, Stoney Creek, Hamilton Mountain) that would be happy to receive you.
Visit our FAQ page to find useful information before your first appointment!